Effects of Consanguineous Marriage on Pregnancy Outcome in Rural Areas of Theni District –A Comparative and Descriptive Study.
Main Article Content
Abstract
Objectives:
To assess the effects of consanguineous marriage on pregnancy outcome.
To compare the effects of consanguineous and nonconsanguineous marriage on pregnancy outcome.
To identify the association between the effects of consanguineous marriage with degree, age, relegion, sex of the baby and birth order.
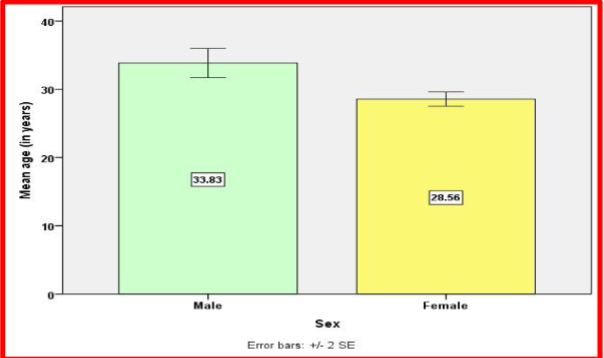
Methodology: Nonrandomized convenient sampling technique was used to select the samples of 160 women and men between the age group of 15-60.
Result: Consanguineous married mothers are having 17.07% of Congenital anomaly/abortion/still birth whereas Non consanguineous mothers are having only 2.56% Consanguineous married mothers are having 21.95% of Genetic disorders whereas Non consanguineous mothers are having only 3.85% Consanguineous married mothers are having 60.98% of healthy pregnancy outcome whereas Non consanguineous mothers are having 93.59%. This difference is statistically significant. Statistically there is a significant difference between Consanguineous and nonConsanguineous married mothers pregnancy outcome. It was observed using chi square test. Consanguineous married mothers are having 9.3 times risk of having pregnancy outcome problems. . It was observed using odds ratio with 95% confidence interval.
Article Details
References
Adele Pillitteri, Maternal and Child health Nursing, 5th ed, Philadelphia. 2007:147 – 164.
Carole Kenner, Judy Weight Lott, Comprehensive Neonatal Nursing,3rd ed .Soundars Company, Philadelphia:2004
Patwari,A.k,. H.P.S. Sachdev Frontiers in Social Paediatrics. Jaypee brothers medical publishers (P) ltd, New Delhi:2002
Polit andHungelr,Nursing Research.5thed, J.P. Lippincott publishers, Philadelphia:1999
Ronald. S. Illing worth. The Development of the infant and young child “Normal and abnormal” 9th ed, Churchill Livingstone, London: 2004
Anand k Sagar et al.,Consanguinety and child health. Community Genetics.2008;32:431-437..
Antony D.K. Enabling mothers to ensure health of new borns. Health Action. Nov 2002:9-12.
Bittles, A. H., & Black, M.L.The impact of consanguinity on neonatal and infant health. Early Human Development.2010;86(11): 737-741
Gowda, R. S., & Ramachandra, N.B. Parental consanguinity increases congenital heart diseases in South India, Annals of human biology.2006:33 (5-6): 519-528.
Oehler J.M, Hannan.T et al.,Maternal views of preterm infants and responsiveness to social interaction. Neanatology Network;2004 Sep: 12(6); 67-74
Partridge J.C. Martinez .A.M. International comparison of care for preterm infants; parents perceptions of counseling and decision making. Journal of pediatrics; 2005: Aug : 116(2);263-71
Preyde. M. Ardal .F. Effectiveness of a parent “Buddy” Program for mothers of very preterm infants in a NICU. Indian academic of paediatrics.2006:5;168(8); 968-73.
Slusher.T , Hampton. R et al., Promoting care for hospitalized low birth weight and preterm infants in Nigeria-A feasibility study. Pediatrics Today; 2005:19(2)191-198.
WHO.The World Health Report: 2010; Geneva: World Health Organization. Yunis, K., El Rafei, et al.,
Peri natal outcomes and prevention-a view from the Middle East. Neo Reviews: 2008;9(2):59.
Alsuwaida, N (2016) Women’s education in Saudi Arabia. Journal of International Educational Research 12(4), 111–118.Google Scholar
Bakoush, O, Nicholls, M and Denic, S (2016) Selection of kin for spouse: importance of socioeconomic status, reputation and beauty. Journal of King Saud University – Science 28(4), 286– 292.CrossRefGoogle Scholar.
El-Mouzan, M, Al-Salloum, A, Al-Hebish, A, Qurachi, M and Al-Omar, A (2007) Regional variations in the prevalence of consanguinity in Saudi Arabia. Saudi Medical Journal 28(12), 1881–1884.Google ScholarPubMed
General Authority for Statistics (2016) Demographic Research Bulletin, p. 204.
URL: https://www.stats.gov.sa/sites/default/files/ar-demographic-research-2016_5.pdf (accessed 20th September 2017).Google Scholar.
Hamamy, H (2012) Consanguineous marriages. Preconception consultation in primary health care settings. Journal of Community Genetics 3, 185–192.CrossRefGoogle ScholarPubMed
Islam, MM, Ababneh, FM and Khan, MH (2018) Consanguineous marriage in Jordan: an update. Journal of Biosocial Science 50(4), 573–578.CrossRefGoogle ScholarPubMed
Jaouad, I, Elalaqui, S, Spiti, A and Elkerh, F (2009) Consanguineous marriages in Morocco and the consequence for the incidence of autosomal recessive disorders. Journal of Biosocial Science 41(5), 575–581.CrossRefGoogle ScholarPubMed
Joseph, N, Pavan, K, Ganapathi, K, Apoorva, P, Sharma, P and Jhamb, J (2015) Health awareness and consequences of consanguineous marriages. Journal of Primary Care & Community Health 6(2), 121– 127.CrossRefGoogle ScholarPubMed
Nouri, N, Nouri, N, Tirgar, S, Solimani, E, Yazdani, V, Zahedi, F and Larjeni, B (2017) Consanguineou s marriages in the genetic counseling centers of Isfahan and the ethical issues of clinical consultations. Journal of Medical Ethics and History of Medicine 10(1), 10.Google ScholarPubMed
Saeed, U and Piracha, Z (2016) Thalassemia: impact of consanguineous marriages on most prevalent monogenic disorders of humans. Asian Pacific Journal of Tropical Disease 6(10), 837– 840.CrossRefGoogle Scholar
Warsy, A, Al-Jaser, M, Albdass, A, Al-Daihan, S and Alanzi, M (2014) Is consanguinity prevalence decreasing in Saudis? A study in two generations. African Health Sciences 14(2), 314– 321.CrossRefGoogle ScholarPubMed
Zaini, R (2016) Sickle-cell anemia and consanguinity among the Saudi Arabian population. Archives