A Study of Relationship Between Hypothyrodism with Central Obesity
Main Article Content
Abstract
Background: The precise estimation of the prevalence of important cardiovascular risk factors is of great interest. In order to evaluate the health and nutritional status of “adults and children in the United States”, a series of studies known as the “National Health and Nutrition Examination Survey (NHANES)” was created.
Aim and Objective: To study the co-relation of hypothyrodism with central obesity.
Methodology: The present study was conducted in the “OPD of General Medicine, Santosh medical college and hospital, Ghaziabad, Uttar Pradesh”. In their regular clinical practise, these data would have prognostic significance and consequences for clinicians and to establish strategies for improved treatment of their patients.
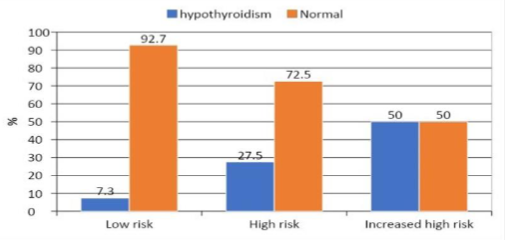
Result: On the basis of the IDF criteria for central obesity for the diagnosis, a total of 100 individuals with old and newly diagnosed metabolic syndrome were evaluated. More than half of patients were “females (56%)” and the “prevalence of hypothyroidism” was “higher among female patients (25%) than males (15.9%)”.
Conclusion: The main conclusion of this study was that, in study participants with hypothyroidism, there is a substantial link between “thyroid homeostasis and obesity”. In order to the best of our knowledge, only a few research have attempted to assess individuals with hypothyroidism utilising a sizable, “community-based sample” in order to discover a separate relationship between hypothyrodism and central obesity indices.
Article Details
References
O'Neill S., O'Driscoll L. Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obesity Reviews. 2015;16(1):1 12.
Palmer MK and Toth PP. Trends in lipids, obesity, metabolic syndrome, and diabetes mellitus in the United States: an NHANES analysis (2003-2004 to 2013-2104). Obesity 2019; 27: 309 314.
Guan B, Chen YY, Yang W, et al. Effect of bariatric surgery on thyroid function in obese patients: a systematic review and meta-analysis. ObesSurg 2017; 27: 3292 3305.
McAninch EA and Bianco AC. Thyroid hormone signaling in energy homeostasis and energy metabolism. Ann N Y AcadSci 2014; 1311: 77 8
Jiang J, Ahn J, Huang WY, Hayes RB. Association of obesity with cardiovascular disease mortality in the PLCO trial. Prev Med 2013;57:60-64.
Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med 2010;363:2211-2219.
Czernichow S, Kengne AP, Huxley RR, et al. Comparison of waist-to-hip ratio and other obesity indices as predictors of cardiovascular disease risk in people with type-2 diabetes: a prospective cohort study from ADVANCE. Eur J CardiovascPrevRehabil 2011;18:312-319.
Singh M, Arora R, Kodumuri V, Khosla S, Jawad E. Coronary revascularization in diabetic patients: current state of evidence. ExpClinCardiol 2011;16:16-22.
Kaur J. A comprehensive review on metabolic syndrome. Cardiol Res Pract 2014;2014:943162. doi:10.1155/2014/943162
National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143-3421.
Garca-Estevez DA, Araújo-Vilar D, Saavedra-González A, Fiestras-Janeiro G, Cabezas-Cerrato J. Analysis of the relationship between body mass index, insulin resistance, and beta-cell function: a cross-sectional study using the minimal model. Metabolism 2004;53:1462-1466.
Leon BM, Maddox TM. Diabetes and cardiovascular disease: epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes 2015;6:1246-1258.
Matheus AS, Tannus LR, Cobas RA, Palma CC, Negrato CA, Gomes MB. Impact of diabetes on cardiovascular disease: an update. Int J Hypertens 2013;2013:653789. doi:10.1155/2013/653789
P. N. Taylor, D. Albrecht, A. Scholz et al., “Global epidemiology of hyperthyroidism and hypothyroidism,” Nature Reviews Endocrinology, vol. 14, no. 5, pp. 301–316, 2018.
L. T. van Hulsteijn, R. Pasquali, F. Casanueva et al., “Prevalence of endocrine disorders in obese patients: systematic review and meta-analysis,” European Journal of Endocrinology, vol. 182, no. 1, pp. 11–21, 2020.
M.-K. Lee, Y. M. Kim, S.-Y. Sohn, J.-H. Lee, Y. J. Won, and S. H. Kim, “Evaluation of the relationship of subclinical hypothyroidism with metabolic syndrome and its components in adolescents: a population-based study,” Endocrine, vol. 65, no. 3, pp. 608–615, 2019.
Gay JC et al. The Colorado thyroid disease prevalence study. Arch intern med 2000;160:526-534
Deshmukh V, Farishta F, Bhole M. Thyroid Dysfunction in Patients with MetabolicSyndrome: A Cross-Sectional, Epidemiological, Pan-India Study. Int J Endocrinol.2018.
Aljabri KS, Alnasser IM, Bokhari SA, Alshareef MA, Khan PM, et al. The Prevalenceof Hypothyroidism in Patients with Metabolic Syndrome in Saudi Community BasedHospital:ARetrospectiveSingleCentreStudy. IntJDiabetesClinRes2019;6(103).
Meng Z., Liu M., Zhang Q. et al. Gender and age impacts onthe association betweenthyroidfunctionandmetabolicsyndromeinChinese.Medicine2015;94(50).
Tehrani F. R., Tohidi M., and Dovom M. R. A populationbased study on the associationofthyroidstatuswithcomponentsofthemetabolicsyndrome.JournalofDiabetes&Metabolism2011;2(8)